Microfluidics: Rapid Diagnosis for Breast Cancer
Corresponding Author: Suresh Neethirajan
Nano-Micro Letters,
Vol. 8 No. 3 (2016), Article Number: 204-220
Abstract
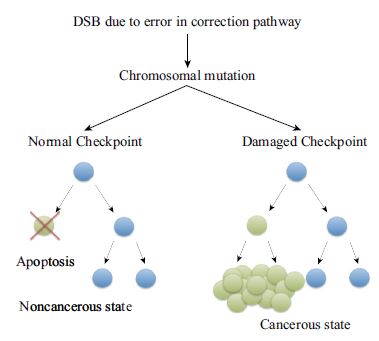
Breast cancer affected 1.7 million people worldwide in 2012 and accounts for approximately 23.3 % of all cancers diagnosed in women. The disease is characterized by a genetic mutation, either inherited or resulting from environmental factors, that causes uncontrollable cellular growth of breast tissue or adjacent tissues. Current means of diagnosing this disease depend on the individual analyzing the results from bulky, highly technical, and expensive equipment that is not globally accessible. As a result, patients can go undiagnosed due to a lack of available equipment or be over-diagnosed due to human error. This review attempts to highlight current means of diagnosing breast cancer and critically analyze their effectiveness and usefulness in terms of patient survival. An alternative means based on microfluidics biomarker detection is then presented. This method can be considered as a primary screening tool for diagnosing breast cancer based on its robustness, high throughput, low energy requirements, and accessibility to the general public.
Keywords
Download Citation
Endnote/Zotero/Mendeley (RIS)BibTeX
- L.A. Torre, F. Bray, R.L. Siegel, J. Ferlay, J. LortetTieulent, A. Jemal, Global cancer statistics, 2012. CA. Cancer J. Clin. 65(2), 87–108 (2015). doi:10.3322/caac.21262
- L.N. Kolonel, D. Altshuler, B.E. Henderson, The multiethnic cohort study: exploring genes, lifestyle and cancer risk. Nat. Rev. Cancer 4(7), 519–527 (2004). doi:10.1038/nrc1389
- J.F. Sallis, J.J. Prochaska, W.C. Taylor, A review of correlates of physical activity of children and adolescents. Med. Sci. Sports Exerc. 32(5), 963–975 (2000). doi:10.1097/00005768-200005000-00014
- R.C. Brownson, T.K. Boehmer, D.A. Luke, Declining rates of physical activity in the United States: what are the contributors? Annu. Rev. Public Health 26, 421–443 (2005). doi:10.1146/annurev.publhealth.26.021304.144437
- S.Y. Kimm, N.W. Glynn, A.M. Kriska, B.A. Barton, S.S. Kronsberg, S.R. Daniels, P.B. Crawford, Z.I. Sabry, K. Liu, Decline in physical activity in black girls and white girls during adolescence. N. Engl. J. Med. 347(10), 709–715 (2002). doi:10.1056/NEJMoa003277
- K.R. Allison, E.M. Adlaf, J.J. Dwyer, D.C. Lysy, H.M. Irving, The decline in physical activity among adolescent students: a cross-national comparison. Can. J. Public Health 98(2), 97–100 (2007)
- S.J. Marshall, S.J. Biddle, T. Gorely, N. Cameron, I. Murdey, Relationships between media use, body fatness and physical activity in children and youth: a meta-analysis. Int. J. Obes. 28(10), 1238–1246 (2004). doi:10.1038/sj.ijo.0802706
- R. Sturm, A. Hattori, Morbid obesity rates continue to rise rapidly in the United States. Int. J. Obes. 37(6), 889–891 (2013). doi:10.1038/ijo.2012.159
- C.L. Ogden, M.D. Carroll, B.K. Kit, K.M. Flegal, Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 311(8), 806–814 (2014). doi:10.1001/jama.2014.732
- H. Pan, R.G. Gray, E.B.C.T.C. Group, Effect of obesity in premenopausal ER+ early breast cancer: EBCTCG data on 80,000 patients in 70 trials. J. Clin. Oncol. (Meeting Abstracts), 32(15_ suppl 503) (2014)
- R.S. Cecchini, J.P. Costantino, J.A. Cauley, W.M. Cronin, D.L. Wickerham, S.R. Land, J.L. Weissfeld, N. Wolmark, Body mass index and the risk for developing invasive breast cancer among high-risk women in NSABP P-1 and STAR breast cancer prevention trials. Cancer Prev. Res. 5(4), 583–592 (2012). doi:10.1158/1940-6207.CAPR-11-0482
- F.A. Sinicrope, A.J. Dannenberg, Obesity and breast cancer prognosis: weight of the evidence. J. Clin. Oncol. 29(1), 4–7 (2011). doi:10.1200/JCO.2010.32.1752
- F. Hjern, A. Wolk, N. Håkansson, Obesity, physical inactivity, and colonic diverticular disease requiring hospitalization in women: a prospective cohort study. Am. J. Gastroenterol. 107(2), 296–302 (2012). doi:10.1038/ajg.2011.352
- S.L. Murphy, J. Xu, K.D. Kochanek, Deaths: final data for 2010. national vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics. Natl. Vital Stat. Syst. 61(4), 1–117 (2013)
- K. Kochanek, S. Murphy, R. Anderson, C. Scott, Deaths: Final Data for 2002. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics. Natl. Vital Stat. Syst. 53(5), 1–115 (2004)
- C.L. Carter, C. Allen, D.E. Henson, Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer 63(1), 181–187 (1989). doi:10.1002/1097-0142(19890101)63:1<181:AID-CNCR2820630129>3.0.CO;2-H
- A. Jemal, R. Siegel, E. Ward, Y. Hao, J. Xu, T. Murray, M.J. Thun, Cancer statistics, 2008. CA. Cancer J. Clin. 58(2), 71–96 (2008). doi:10.3322/CA.2007.0010
- R. Siegel, C. DeSantis, A. Jemal, Colorectal cancer statistics, 2014. CA. Cancer J. Clin. 64(2), 104–117 (2014). doi:10.3322/caac.21220
- P. Boyle, B. Levin (eds.), World Cancer Report 2008 (International Agency for Research on Cancer (IARC) press, Lyon, 2008)
- A.C. Society, Breast Cancer Survival Rates, By Stage. http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-survival-by-stage
- M. Esebua, Cell and molecular biology of breast cancer, in Histopathology and Grading of Breast Cancer, ed. by H. Schatten (Springer, New York, 2013), pp. 1–27. doi:10.1007/978-1-62703-634-4_1
- C. Li, D. Uribe, J. Daling, Clinical characteristics of different histologic types of breast cancer. Br. J. Cancer. 93(9), 1046–1052 (2005). doi:10.1038/sj.bjc.6602787
- T. Korhonen, T. Kuukasjärvi, H. Huhtala, E.-L. Alarmo, K. Holli, A. Kallioniemi, L. Pylkkänen, The impact of lobular and ductal breast cancer histology on the metastatic behavior and long term survival of breast cancer patients. Breast 22(6), 1119–1124 (2013). doi:10.1016/j.breast.2013.06.001
- B. Weigelt, J.L. Peterse, L.J. Van’t, Veer, Breast cancer metastasis: markers and models. Nat. Rev. Cancer 5(8), 591–602 (2005). doi:10.1038/nrc1670
- P.J. Stephens, P.S. Tarpey, H. Davies, P. Van Loo, C. Greenman, D.C. Wedge, S. Nik-Zainal, S. Martin, I. Varela, G.R. Bignell, The landscape of cancer genes and mutational processes in breast cancer. Nature 486(7403), 400–404 (2012). doi:10.1038/nature11017
- S. Nik-Zainal, L.B. Alexandrov, D.C. Wedge, P. Van Loo, C.D. Greenman et al., Mutational processes molding the genomes of 21 breast cancers. Cell 149(5), 979–993 (2012). doi:10.1016/j.cell.2012.04.024
- H. Dvinge, A. Git, S. Gräf, M. Salmon-Divon, C. Curtis et al., The shaping and functional consequences of the microRNA landscape in breast cancer. Nature 497(7449), 378–382 (2013). doi:10.1038/nature12108
- H. Nakajima, Y. Ishikawa, M. Furuya, T. Sano, Y. Ohno, J. Horiguchi, T. Oyama, Protein expression, gene amplification, and mutational analysis of EGFR in triple-negative breast cancer. Breast Cancer 21(1), 66–74 (2014). doi:10.1007/s12282-012-0354-1
- Cancer Genome Atlas Network, Comprehensive molecular portraits of human breast tumours. Nature 490(7418), 61–70 (2012). doi:10.1038/nature11412
- K.W. Caestecker, G.R. Van de Walle, The role of BRCA1 in DNA double-strand repair: past and present. Exp. Cell Res. 319(5), 575–587 (2013). doi:10.1016/j.yexcr.2012.11.013
- L. Robertson, H. Hanson, S. Seal, M. Warren-Perry, D. Hughes et al., BRCA1 testing should be offered to individuals with triple-negative breast cancer diagnosed below 50 years. Br. J. Cancer 106(6), 1234–1238 (2012). doi:10.1038/bjc.2012.31
- N. Tung, C. Battelli, B. Allen, R. Kaldate, S. Bhatnagar et al., Frequency of mutations in individuals with breast cancer referred for BRCA1 and BRCA2 testing using next-generation sequencing with a 25-gene panel. Cancer 121(1), 25–33 (2015). doi:10.1002/cncr.29010
- N. Tung, J.E. Garber, A. Lincoln, S.M. Domchek, Frequency of triple-negative breast cancer in BRCA1 mutation carriers: comparison between common Ashkenazi Jewish and other mutations. J. Clin. Oncol. 30(35), 4447–4448 (2012). doi:10.1200/JCO.2012.44.5635
- K.M. Kuusisto, A. Bebel, M. Vihinen, J. Schleutker, S.-L. Sallinen, Screening for BRCA1, BRCA2, CHEK2, PALB2, BRIP1, RAD50, and CDH1 mutations in high-risk Finnish BRCA1/2-founder mutation-negative breast and/or ovarian cancer individuals. Breast Cancer Res. 13(1), R20 (2011). doi:10.1186/bcr2832
- S.N. Powell, L.A. Kachnic, Roles of BRCA1 and BRCA2 in homologous recombination, DNA replication fidelity and the cellular response to ionizing radiation. Oncogene 22(37), 5784–5791 (2003). doi:10.1038/sj.onc.1206678
- S.F. Bunting, E. Callén, M.L. Kozak, J.M. Kim, N. Wong et al., BRCA1 functions independently of homologous recombination in DNA interstrand crosslink repair. Mol. Cell 46(2), 125–135 (2012). doi:10.1016/j.molcel.2012.02.015
- M.S. Brose, T.C. Smyrk, B. Weber, H.T. Lynch, Holland–Frei cancer medicine, in Genetic Predisposition to Cancer, Chap. 16, 6th edn., ed. by D.W. Kufe, R.E. Pollock, R.R. Weichselbaum, et al. (American Cancer Society, Hamilton, 2003). doi:10.1007/978-1-62703-634-4_1
- D.T. Long, J.C. Walter, A novel function for BRCA1 in crosslink repair. Mol. Cell 46(2), 111–112 (2012). doi:10.1016/j.molcel.2012.04.010
- S.B. Cantor, D.W. Bell, S. Ganesan, E.M. Kass, R. Drapkin et al., BACH1, a novel helicase-like protein, interacts directly with BRCA1 and contributes to its DNA repair function. Cell 105(1), 149–160 (2001). doi:10.1016/S0092-8674(01)00304-X
- M.W. Wong, C. Nordfors, D. Mossman, G. Pecenpetelovska, K.A. Avery-Kiejda, B. Talseth-Palmer, N.A. Bowden, R.J. Scott, BRIP1, PALB2, and RAD51C mutation analysis reveals their relative importance as genetic susceptibility factors for breast cancer. Breast Cancer Res. Treat. 127(3), 853–859 (2011). doi:10.1007/s10549-011-1443-0
- R. Buisson, J. Niraj, J. Pauty, R. Maity, W. Zhao, Y. Coulombe, P. Sung, J.-Y. Masson, Breast cancer proteins PALB2 and BRCA2 stimulate polymerase h in recombination-associated DNA synthesis at blocked replication forks. Cell Rep. 6(3), 553–564 (2014). doi:10.1016/j.celrep.2014.01.009
- N. Rahman, S. Seal, D. Thompson, P. Kelly, A. Renwick et al., PALB2, which encodes a BRCA2-interacting protein, is a breast cancer susceptibility gene. Nat. Genet. 39(2), 165–167 (2007). doi:10.1038/ng1959
- W.L. Bridge, C.J. Vandenberg, R.J. Franklin, K. Hiom, The BRIP1 helicase functions independently of BRCA1 in the Fanconi anemia pathway for DNA crosslink repair. Nat. Genet. 37(9), 953–957 (2005). doi:10.1038/ng1627
- P.-L. Chen, C.-F. Chen, Y. Chen, J. Xiao, Z.D. Sharp, W.-H. Lee, The BRC repeats in BRCA2 are critical for RAD51 binding and resistance to methyl methanesulfonate treatment. PNAS 95(9), 5287–5292 (1998). doi:10.1073/pnas.95.9.5287
- A. Carreira, S.C. Kowalczykowski, Two classes of BRC repeats in BRCA2 promote RAD51 nucleoprotein filament function by distinct mechanisms. PNAS 108(26), 10448–10453 (2011). doi:10.1073/pnas.1106971108
- S. Woditschka, D. Palmieri, R. Duchnowska, J. Jassem, S. Badve, G.W. Sledge, P.S. Steeg, Overexpression of RAD51 promotes brain metastases from breast cancer. Cancer Res. 73(8 Suppl.), 4589 (2013). doi:10.1158/1538-7445.AM2013-4589
- H.L. Klein, The consequences of Rad51 overexpression for normal and tumor cells. DNA Repair 7(5), 686–693 (2008). doi:10.1016/j.dnarep.2007.12.008
- J.-Y. Park, T.R. Singh, N. Nassar, F. Zhang, M. Freund, H. Hanenberg, A.R. Meetei, P.R. Andreassen, Breast cancer-associated missense mutants of the PALB2 WD40 domain, which directly binds RAD51C, RAD51 and BRCA2, disrupt DNA repair. Oncogene 33(40), 4803–4812 (2013). doi:10.1038/onc.2013.421
- R. Hashizume, M. Fukuda, I. Maeda, H. Nishikawa, D. Oyake, Y. Yabuki, H. Ogata, T. Ohta, The RING heterodimer BRCA1-BARD1 is a ubiquitin ligase inactivated by a breast cancer-derived mutation. J. Biol. Chem. 276(18), 14537–14540 (2001). doi:10.1074/jbc.C000881200
- D. Lisa, S. Daniela, Y.S. Simone, K. Julia, W. Lisa, BRCA1-mediated repression of mutagenic end-joining of DNA double-strand breaks requires complex formation with BACH1. Biochem. J. 441(3), 919–926 (2012). doi:10.1042/BJ20110314
- R. Parsons, L. Simpson, PTEN and cancer, in Tumor Suppressor Genes Volume 1: Pathways and Isolation Strategies, ed. by W.S. El-Deiry (Springer, New York, 2003), pp. 147–166. doi:10.1385/1-59259-328-3:147
- J. Li, C. Yen, D. Liaw, K. Podsypanina, S. Bose et al., PTEN, a putative protein tyrosine phosphatase gene mutated in human brain, breast, and prostate cancer. Science 275(5308), 1943–1947 (1997). doi:10.1126/science.275.5308.1943
- L.-P. Weng, W.M. Smith, P.L. Dahia, U. Ziebold, E. Gil, J.A. Lees, C. Eng, PTEN suppresses breast cancer cell growth by phosphatase activity-dependent G1 arrest followed by cell death. Cancer Res. 59(22), 5808–5814 (1999)
- P.L. Depowski, S.I. Rosenthal, J.S. Ross, Loss of expression of the PTEN gene protein product is associated with poor outcome in breast cancer. Mod. Pathol. 14(7), 672–676 (2001). doi:10.1038/modpathol.3880371
- A. Carracedo, A. Alimonti, P.P. Pandolfi, PTEN level in tumor suppression: how much is too little? Cancer Res. 71(3), 629–633 (2011). doi:10.1158/0008-5472.CAN-10-2488
- M.S. Song, L. Salmena, P.P. Pandolfi, The functions and regulation of the PTEN tumour suppressor. Nat. Rev. Mol. Cell Biol. 13(5), 283–296 (2012). doi:10.1038/nrm3330
- E.-S.A. Arafa, Q. Zhu, Z.I. Shah, G. Wani, B.M. Barakat, I. Racoma, M.A. El-Mahdy, A.A. Wani, Thymoquinone up-regulates PTEN expression and induces apoptosis in doxorubicin-resistant human breast cancer cells. Mutat. Res./Fundam. Mol. Mech. Mutagen. 706(1), 28–35 (2011). doi:10.1016/j.mrfmmm.2010.10.007
- A. Bononi, M. Bonora, S. Marchi, S. Missiroli, F. Poletti, C. Giorgi, P. Pandolfi, P. Pinton, Identification of PTEN at the ER and MAMs and its regulation of Ca2+ signaling and apoptosis in a protein phosphatase-dependent manner. Cell Death Differ. 20(12), 1631–1643 (2013). doi:10.1038/cdd.2013.77
- M. Unseld, A. Chilla, C. Pausz, J. Breuss, G. Schabbauer, G. Prager, PTEN dependent angiogenesis is mainly regulated by (tumor secreted-) uPAR. Cancer Res. 74(19 Suppl.), 3602 (2014). doi:10.1158/1538-7445.AM2014-3602
- S. Mondal, K.K. Subramanian, J. Sakai, B. Bajrami, H.R. Luo, Phosphoinositide lipid phosphatase SHIP1 and PTEN coordinate to regulate cell migration and adhesion. Mol. Biol. Cell 23(7), 1219–1230 (2012). doi:10.1091/mbc.E11-10-0889
- M. Tamura, J. Gu, K. Matsumoto, S.-I. Aota, R. Parsons, K.M. Yamada, Inhibition of cell migration, spreading, and focal adhesions by tumor suppressor PTEN. Science 280(5369), 1614–1617 (1998). doi:10.1126/science.280.5369.1614
- K.M. Yamada, M. Araki, Tumor suppressor PTEN: modulator of cell signaling, growth, migration and apoptosis. J. Cell Sci. 114(13), 2375–2382 (2001). doi:10.1083/jcb.143.5.1375
- L. Ma, J. Teruya-Feldstein, R.A. Weinberg, Tumour invasion and metastasis initiated by microRNA-10b in breast cancer. Nature 449(7163), 682–688 (2007). doi:10.1038/nature06174
- M.V. Iorio, M. Ferracin, C.-G. Liu, A. Veronese, R. Spizzo et al., MicroRNA gene expression deregulation in human breast cancer. Cancer Res. 65(16), 7065–7070 (2005). doi:10.1158/0008-5472.CAN-05-1783
- L.-X. Yan, X.-F. Huang, Q. Shao, M.-Y. Huang, L. Deng, Q.-L. Wu, Y.-X. Zeng, J.-Y. Shao, MicroRNA miR-21 overexpression in human breast cancer is associated with advanced clinical stage, lymph node metastasis and patient poor prognosis. RNA 14(11), 2348–2360 (2008). doi:10.1261/rna.1034808
- M.V. Iorio, P. Casalini, C. Piovan, G. Di Leva, A. Merlo, T. Triulzi, S. Ménard, C.M. Croce, E. Tagliabue, microrna-205 regulates HER3 in human breast cancer. Cancer Res. 69(6), 2195–2200 (2009). doi:10.1158/0008-5472.CAN-08-2920
- F. Yu, H. Yao, P. Zhu, X. Zhang, Q. Pan, C. Gong, Y. Huang, X. Hu, F. Su, J. Lieberman, let-7 regulates self renewal and tumorigenicity of breast cancer cells. Cell 131(6), 1109–1123 (2007). doi:10.1016/j.cell.2007.10.054
- R. Liu, X. Wang, G.Y. Chen, P. Dalerba, A. Gurney et al., The prognostic role of a gene signature from tumorigenic breast-cancer cells. N. Engl. J. Med. 356(3), 217–226 (2007). doi:10.1056/NEJMoa063994
- Y. Lee, V.N. Kim, In vitro and in vivo assays for the activity of Drosha complex. Methods Enzymol. 427, 87–106 (2007). doi:10.1016/S0076-6879(07)27005-3
- H.M. Heneghan, N. Miller, A.J. Lowery, K.J. Sweeney, J. Newell, M.J. Kerin, Circulating microRNAs as novel minimally invasive biomarkers for breast cancer. Ann. Surg. 251(3), 499–505 (2010). doi:10.1097/SLA.0b013e3181cc939f
- E. O’Day, A. Lal, MicroRNAs and their target gene networks in breast cancer. Breast Cancer Res. 12(2), 201 (2010). doi:10.1186/bcr2484
- S. Sethi, A. Ahmad, S. Mittal, R. Ali, W. Chen, F.H. Sarkar, Upregulation of miR-10b associated with breast cancer metastasis to brain. Cancer Res. 73(8 Suppl.), 5327 (2013). doi:10.1158/1538-7445.AM2013-5327
- L.B. Frankel, N.R. Christoffersen, A. Jacobsen, M. Lindow, A. Krogh, A.H. Lund, Programmed cell death 4 (PDCD4) is an important functional target of the microRNA miR-21 in breast cancer cells. J. Biol. Chem. 283(2), 1026–1033 (2008). doi:10.1074/jbc.M707224200
- P. Gasparini, F. Lovat, M. Fassan, L. Casadei, L. Cascione et al., Protective role of miR-155 in breast cancer through RAD51 targeting impairs homologous recombination after irradiation. PNAS 111(12), 4536–4541 (2014). doi:10.1073/pnas.1402604111
- P.C. Gøtzsche, M. Nielsen, L. Casadei, Screening for breast cancer with mammography. Cochrane Database Syst. Rev. 1, CD001877 (2011). doi:10.1002/14651858.CD001877.pub4
- E.S. de Paredes (ed.), Atlas of Mammography, 3rd edn. (Lippincott Williams & Wilkins, Philadelphia, 2007)
- C.E.C. Marie Tartar, M.S. Kipper (eds.). Breast Cancer Imaging: A Multidisciplinary, Multimodality Approach (Mosby Elsevier, Philadelphia, PA, 2008)
- J.G. Herman, J.R. Graff, S. Myöhänen, B.D. Nelkin, S.B. Baylin, Methylation-specific PCR: a novel PCR assay for methylation status of CpG islands. PNAS 93(18), 9821–9826 (1996). doi:10.1073/pnas.93.18.9821
- A.E. Hoffman, T. Zheng, C. Yi, D. Leaderer, J. Weidhaas, F. Slack, Y. Zhang, T. Paranjape, Y. Zhu, microRNA miR-196a-2 and breast cancer: a genetic and epigenetic association study and functional analysis. Cancer Res. 69(14), 5970–5977 (2009). doi:10.1158/0008-5472.CAN-09-0236
- D.C. Sgroi, S. Teng, G. Robinson, R. LeVangie, J.R. Hudson, A.G. Elkahloun, In vivo gene expression profile analysis of human breast cancer progression. Cancer Res. 59(22), 5656–5661 (1999)
- S. Paik, G. Tang, S. Shak, C. Kim, J. Baker et al., Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor–positive breast cancer. J. Clin. Oncol. 24(23), 3726–3734 (2006). doi:10.1200/JCO.2005.04.7985
- D. Ford, D. Easton, M. Stratton, S. Narod, D. Goldgar et al., Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. Am. J. Hum. Genet. 62(3), 676–689 (1998). doi:10.1086/301749
- J.S. Reis-Filho, L. Pusztai, Gene expression profiling in breast cancer: classification, prognostication, and prediction. Lancet 378(9805), 1812–1823 (2011). doi:10.1016/S0140-6736(11)61539-0
- M.A. Innis, D.H. Gelfand, J.J. Sninsky, T.J. White (eds.), PCR Protocols: A Guide to Methods and Applications (Academic Press, San Diego, 2012)
- E. Evron, W.C. Dooley, C.B. Umbricht, D. Rosenthal, N. Sacchi et al., Detection of breast cancer cells in ductal lavage fluid by methylation-specific PCR. Lancet 357(9265), 1335–1336 (2001). doi:10.1016/S0140-6736(00)04501-3
- M. Ignatiadis, G. Kallergi, M. Ntoulia, M. Perraki, S. Apostolaki et al., Prognostic value of the molecular detection of circulating tumor cells using a multimarker reverse transcription-PCR assay for cytokeratin 19, mammaglobin A, and HER2 in early breast cancer. Clin. Cancer Res. 14(9), 2593–2600 (2008). doi:10.1158/1078-0432.CCR-07-4758
- M.J. Fackler, M. McVeigh, J. Mehrotra, M.A. Blum, J. Lange, A. Lapides, E. Garrett, P. Argani, S. Sukumar, Quantitative multiplex methylation-specific PCR assay for the detection of promoter hypermethylation in multiple genes in breast cancer. Cancer Res. 64(13), 4442–4452 (2004). doi:10.1158/0008-5472.CAN-03-3341
- T. Fehm, O. Hoffmann, B. Aktas, S. Becker, E.F. Solomayer, D. Wallwiener, R. Kimmig, S. Kasimir-Bauer, Detection and characterization of circulating tumor cells in blood of primary breast cancer patients by RT-PCR and comparison to status of bone marrow disseminated cells. Breast Cancer Res. 11(4), R59 (2009). doi:10.1186/bcr2349
- K. Cuk, M. Zucknick, J. Heil, D. Madhavan, S. Schott et al., Circulating microRNAs in plasma as early detection markers for breast cancer. Int. J. Cancer 132(7), 1602–1612 (2013). doi:10.1002/ijc.27799
- A. Mangolini, M. Ferracin, M.V. Zanzi, E. Saccenti, S.O. Ebnaof et al., Diagnostic and prognostic microRNAs in the serum of breast cancer patients measured by droplet digital PCR. Biomarker Res. 3(1), 12 (2015). doi:10.1186/s40364-015-0037-0
- S. Asaga, C. Kuo, T. Nguyen, M. Terpenning, A.E. Giuliano, D.S. Hoon, Direct serum assay for microRNA-21 concentrations in early and advanced breast cancer. Clin. Chem. 57(1), 84–91 (2011). doi:10.1373/clinchem.2010.151845
- E.S. Lianidou, A. Markou, Circulating tumor cells in breast cancer: detection systems, molecular characterization, and future challenges. Clin. Chem. 57(9), 1242–1255 (2011). doi:10.1373/clinchem.2011.165068
- C. Kretschmer, A. Sterner-Kock, F. Siedentopf, W. Schoenegg, P.M. Schlag, W. Kemmner, Identification of early molecular markers for breast cancer. Mol. Cancer 10(1), 15 (2011). doi:10.1186/1476-4598-10-15
- T.W. Jacobs, A.M. Gown, H. Yaziji, M.J. Barnes, S.J. Schnitt, Comparison of fluorescence in situ hybridization and immunohistochemistry for the evaluation of HER-2/neu in breast cancer. J. Clin. Oncol. 17(7), 1974 (1999)
- A.A. Onitilo, J.M. Engel, R.T. Greenlee, B.N. Mukesh, Breast cancer subtypes based on ER/PR and Her2 expression: comparison of clinicopathologic features and survival. Clin. Med. Res. 7(1–2), 4–13 (2009). doi:10.3121/cmr.2008.825
- W. Saadi, S.-J. Wang, F. Lin, N.L. Jeon, A parallel-gradient microfluidic chamber for quantitative analysis of breast cancer cell chemotaxis. Biomed. Microdevices 8(2), 109–118 (2006). doi:10.1007/s10544-006-7706-6
- H.W. Hou, Q. Li, G. Lee, A. Kumar, C. Ong, C.T. Lim, Deformability study of breast cancer cells using microfluidics. Biomed. Microdevices 11(3), 557–564 (2009). doi:10.1007/s10544-008-9262-8
- K.W. Kwon, S.S. Choi, S.H. Lee, B. Kim, S.N. Lee, M.C. Park, P. Kim, S.Y. Hwang, K.Y. Suh, Label-free, microfluidic separation and enrichment of human breast cancer cells by adhesion difference. Lab on a Chip 7(11), 1461–1468 (2007). doi:10.1039/b710054j
- M.J. Van De Vijver, Y.D. He, L.J. van’t Veer, H. Dai, A.A. Hart, A gene-expression signature as a predictor of survival in breast cancer. N. Engl. J. Med. 347(25), 1999–2009 (2002). doi:10.1056/NEJMoa021967
- J. Knight, Microfluidics: Honey. I shrunk the lab. Nature 418(6897), 474–475 (2002). doi:10.1038/418474a
- J. Chen, D. Chen, Y. Xie, T. Yuan, X. Chen, Progress of microfluidics for biology and medicine. Nano-Micro Lett. 5(1), 66–80 (2013). doi:10.1007/BF03354852
- J. Chen, J. Li, Y. Sun, Microfluidic approaches for cancer cell detection, characterization, and separation. Lab Chip 12(10), 1753–1767 (2012). doi:10.1039/c2lc21273k
- T.A. Nguyen, T.-I. Yin, D. Reyes, G.A. Urban, Microfluidic chip with integrated electrical cell-impedance sensing for monitoring single cancer cell migration in three-dimensional matrixes. Anal. Chem. 85(22), 11068–11076 (2013). doi:10.1021/ac402761s
- J.W. Song, S.P. Cavnar, A.C. Walker, K.E. Luker, M. Gupta, Y.-C. Tung, G.D. Luker, S. Takayama, Microfluidic endothelium for studying the intravascular adhesion of metastatic breast cancer cells. PloS One 4(6), e5756 (2009). doi:10.1371/journal.pone.0005756
- A.T.-H. Hsieh, P.J.-H. Pan, A.P. Lee, Rapid label-free DNA analysis in picoliter microfluidic droplets using FRET probes. Microfluid. Nanofluid 6(3), 391–401 (2009). doi:10.1007/s10404-009-0406-9
- K.A. Mangold, V. Wang, S.M. Weissman, W.S. Rubinstein, K.L. Kaul, Detection of BRCA1 and BRCA2 Ashkenazi Jewish founder mutations in formalin-fixed paraffin-embedded tissues using conventional PCR and heteroduplex/amplicon size differences. J. Mol. Diagn. 12(1), 20–26 (2010). doi:10.2353/jmoldx.2010.090023
- A. Rasooly, J. Jacobson, Development of biosensors for cancer clinical testing. Biosens. Bioelectron. 21(10), 1851–1858 (2006). doi:10.1016/j.bios.2006.01.003
- J. van Mameren, M. Modesti, R. Kanaar, C. Wyman, E.J. Peterman, G.J. Wuite, Counting RAD51 proteins disassembling from nucleoprotein filaments under tension. Nature 457(7230), 745–748 (2009). doi:10.1038/nature07581
- S. Vorwerk, K. Ganter, Y. Cheng, J. Hoheisel, P.F. Stähler, M. Beier, Microfluidic-based enzymatic on-chip labeling of miRNAs. New Biotechnol. 25(2), 142–149 (2008). doi:10.1016/j.nbt.2008.08.005
- F. Moltzahn, A.B. Olshen, L. Baehner, A. Peek, L. Fong, H. Stöppler, J. Simko, J.F. Hilton, P. Carroll, R. Blelloch, Microfluidic-based multiplex qRT-PCR identifies diagnostic and prognostic microRNA signatures in the sera of prostate cancer patients. Cancer Res. 71(2), 550–560 (2011). doi:10.1158/0008-5472.CAN-10-1229
- J.S. Jang, V.A. Simon, R.M. Feddersen, F. Rakhshan, D.A. Schultz, M.A. Zschunke, W.L. Lingle, C.P. Kolbert, J. Jen, Quantitative miRNA expression analysis using fluidigm microfluidics dynamic arrays. BMC Genomics 12(1), 144 (2011). doi:10.1186/1471-2164-12-144
- R. Fan, O. Vermesh, A. Srivastava, B.K. Yen, L. Qin et al., Integrated barcode chips for rapid, multiplexed analysis of proteins in microliter quantities of blood. Nat. Biotechnol. 26(12), 1373–1378 (2008). doi:10.1038/nbt.1507
- M. Hu, J. Yan, Y. He, H. Lu, L. Weng, S. Song, C. Fan, L. Wang, Ultrasensitive, multiplexed detection of cancer biomarkers directly in serum by using a quantum dot-based microfluidic protein chip. ACS Nano 4(1), 488–494 (2009). doi:10.1021/nn901404h
- A.F.-J. Jou, C.-H. Lu, Y.-C. He, H. Ou, S.-S. Wang, S.-L. Hsu, I. Willne, J.A. Ho, Diagnosing the miR-141 prostate cancer biomarker using nucleic acid-functionalized CdSe/ZnS QDs and telomerase. Chem. Sci. 6(1), 659–665 (2009). doi:10.1039/C4SC02104E
- J.S. Shim, A.W. Browne, C.H. Ahn, An on-chip whole blood/plasma separator with bead-packed microchannel on COC polymer. Biomed. microdevices 12(5), 949–957 (2010). doi:10.1007/s10544-010-9449-7
- G. Perozziello, P. Candeloro, F. Gentile, A. Nicastri, A. Perri et al., Microfluidics & nanotechnology: towards fully integrated analytical devices for the detection of cancer biomarkers. RSC Adv. 4(98), 55590–55598 (2014). doi:10.1039/C4RA10486B
- C.B. Moelans, P.J. van Diest, Breast: Ductal carcinoma. Atlas Genet. Cytogenet. Oncol. Haematol. 17(3), 209–220 (2012). doi:10.4267/2042/48766
- R.T. Abraham, Cell cycle checkpoint signaling through the ATM and ATR kinases. Genes Dev. 15(17), 2177–2196 (2001). doi:10.1101/gad.914401
- K. Yoshida, Y. Miki, Role of BRCA1 and BRCA2 as regulators of DNA repair, transcription, and cell cycle in response to DNA damage. Cancer Sci. 95(11), 866–871 (2004). doi:10.1111/j.1349-7006.2004.tb02195.x
- K.K. Khanna, S.P. Jackson, DNA double-strand breaks: signaling, repair and the cancer connection. Nat. Genet. 27(3), 247–254 (2001). doi:10.1038/85798
- C. Chen, D.A. Ridzon, A.J. Broomer, Z. Zhou, D.H. Lee et al., Real-time quantification of microRNAs by stem–loop RT–PCR. Nucleic Acids Res. 33(20), e179 (2005). doi:10.1093/nar/gni178
References
L.A. Torre, F. Bray, R.L. Siegel, J. Ferlay, J. LortetTieulent, A. Jemal, Global cancer statistics, 2012. CA. Cancer J. Clin. 65(2), 87–108 (2015). doi:10.3322/caac.21262
L.N. Kolonel, D. Altshuler, B.E. Henderson, The multiethnic cohort study: exploring genes, lifestyle and cancer risk. Nat. Rev. Cancer 4(7), 519–527 (2004). doi:10.1038/nrc1389
J.F. Sallis, J.J. Prochaska, W.C. Taylor, A review of correlates of physical activity of children and adolescents. Med. Sci. Sports Exerc. 32(5), 963–975 (2000). doi:10.1097/00005768-200005000-00014
R.C. Brownson, T.K. Boehmer, D.A. Luke, Declining rates of physical activity in the United States: what are the contributors? Annu. Rev. Public Health 26, 421–443 (2005). doi:10.1146/annurev.publhealth.26.021304.144437
S.Y. Kimm, N.W. Glynn, A.M. Kriska, B.A. Barton, S.S. Kronsberg, S.R. Daniels, P.B. Crawford, Z.I. Sabry, K. Liu, Decline in physical activity in black girls and white girls during adolescence. N. Engl. J. Med. 347(10), 709–715 (2002). doi:10.1056/NEJMoa003277
K.R. Allison, E.M. Adlaf, J.J. Dwyer, D.C. Lysy, H.M. Irving, The decline in physical activity among adolescent students: a cross-national comparison. Can. J. Public Health 98(2), 97–100 (2007)
S.J. Marshall, S.J. Biddle, T. Gorely, N. Cameron, I. Murdey, Relationships between media use, body fatness and physical activity in children and youth: a meta-analysis. Int. J. Obes. 28(10), 1238–1246 (2004). doi:10.1038/sj.ijo.0802706
R. Sturm, A. Hattori, Morbid obesity rates continue to rise rapidly in the United States. Int. J. Obes. 37(6), 889–891 (2013). doi:10.1038/ijo.2012.159
C.L. Ogden, M.D. Carroll, B.K. Kit, K.M. Flegal, Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 311(8), 806–814 (2014). doi:10.1001/jama.2014.732
H. Pan, R.G. Gray, E.B.C.T.C. Group, Effect of obesity in premenopausal ER+ early breast cancer: EBCTCG data on 80,000 patients in 70 trials. J. Clin. Oncol. (Meeting Abstracts), 32(15_ suppl 503) (2014)
R.S. Cecchini, J.P. Costantino, J.A. Cauley, W.M. Cronin, D.L. Wickerham, S.R. Land, J.L. Weissfeld, N. Wolmark, Body mass index and the risk for developing invasive breast cancer among high-risk women in NSABP P-1 and STAR breast cancer prevention trials. Cancer Prev. Res. 5(4), 583–592 (2012). doi:10.1158/1940-6207.CAPR-11-0482
F.A. Sinicrope, A.J. Dannenberg, Obesity and breast cancer prognosis: weight of the evidence. J. Clin. Oncol. 29(1), 4–7 (2011). doi:10.1200/JCO.2010.32.1752
F. Hjern, A. Wolk, N. Håkansson, Obesity, physical inactivity, and colonic diverticular disease requiring hospitalization in women: a prospective cohort study. Am. J. Gastroenterol. 107(2), 296–302 (2012). doi:10.1038/ajg.2011.352
S.L. Murphy, J. Xu, K.D. Kochanek, Deaths: final data for 2010. national vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics. Natl. Vital Stat. Syst. 61(4), 1–117 (2013)
K. Kochanek, S. Murphy, R. Anderson, C. Scott, Deaths: Final Data for 2002. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics. Natl. Vital Stat. Syst. 53(5), 1–115 (2004)
C.L. Carter, C. Allen, D.E. Henson, Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer 63(1), 181–187 (1989). doi:10.1002/1097-0142(19890101)63:1<181:AID-CNCR2820630129>3.0.CO;2-H
A. Jemal, R. Siegel, E. Ward, Y. Hao, J. Xu, T. Murray, M.J. Thun, Cancer statistics, 2008. CA. Cancer J. Clin. 58(2), 71–96 (2008). doi:10.3322/CA.2007.0010
R. Siegel, C. DeSantis, A. Jemal, Colorectal cancer statistics, 2014. CA. Cancer J. Clin. 64(2), 104–117 (2014). doi:10.3322/caac.21220
P. Boyle, B. Levin (eds.), World Cancer Report 2008 (International Agency for Research on Cancer (IARC) press, Lyon, 2008)
A.C. Society, Breast Cancer Survival Rates, By Stage. http://www.cancer.org/cancer/breastcancer/detailedguide/breast-cancer-survival-by-stage
M. Esebua, Cell and molecular biology of breast cancer, in Histopathology and Grading of Breast Cancer, ed. by H. Schatten (Springer, New York, 2013), pp. 1–27. doi:10.1007/978-1-62703-634-4_1
C. Li, D. Uribe, J. Daling, Clinical characteristics of different histologic types of breast cancer. Br. J. Cancer. 93(9), 1046–1052 (2005). doi:10.1038/sj.bjc.6602787
T. Korhonen, T. Kuukasjärvi, H. Huhtala, E.-L. Alarmo, K. Holli, A. Kallioniemi, L. Pylkkänen, The impact of lobular and ductal breast cancer histology on the metastatic behavior and long term survival of breast cancer patients. Breast 22(6), 1119–1124 (2013). doi:10.1016/j.breast.2013.06.001
B. Weigelt, J.L. Peterse, L.J. Van’t, Veer, Breast cancer metastasis: markers and models. Nat. Rev. Cancer 5(8), 591–602 (2005). doi:10.1038/nrc1670
P.J. Stephens, P.S. Tarpey, H. Davies, P. Van Loo, C. Greenman, D.C. Wedge, S. Nik-Zainal, S. Martin, I. Varela, G.R. Bignell, The landscape of cancer genes and mutational processes in breast cancer. Nature 486(7403), 400–404 (2012). doi:10.1038/nature11017
S. Nik-Zainal, L.B. Alexandrov, D.C. Wedge, P. Van Loo, C.D. Greenman et al., Mutational processes molding the genomes of 21 breast cancers. Cell 149(5), 979–993 (2012). doi:10.1016/j.cell.2012.04.024
H. Dvinge, A. Git, S. Gräf, M. Salmon-Divon, C. Curtis et al., The shaping and functional consequences of the microRNA landscape in breast cancer. Nature 497(7449), 378–382 (2013). doi:10.1038/nature12108
H. Nakajima, Y. Ishikawa, M. Furuya, T. Sano, Y. Ohno, J. Horiguchi, T. Oyama, Protein expression, gene amplification, and mutational analysis of EGFR in triple-negative breast cancer. Breast Cancer 21(1), 66–74 (2014). doi:10.1007/s12282-012-0354-1
Cancer Genome Atlas Network, Comprehensive molecular portraits of human breast tumours. Nature 490(7418), 61–70 (2012). doi:10.1038/nature11412
K.W. Caestecker, G.R. Van de Walle, The role of BRCA1 in DNA double-strand repair: past and present. Exp. Cell Res. 319(5), 575–587 (2013). doi:10.1016/j.yexcr.2012.11.013
L. Robertson, H. Hanson, S. Seal, M. Warren-Perry, D. Hughes et al., BRCA1 testing should be offered to individuals with triple-negative breast cancer diagnosed below 50 years. Br. J. Cancer 106(6), 1234–1238 (2012). doi:10.1038/bjc.2012.31
N. Tung, C. Battelli, B. Allen, R. Kaldate, S. Bhatnagar et al., Frequency of mutations in individuals with breast cancer referred for BRCA1 and BRCA2 testing using next-generation sequencing with a 25-gene panel. Cancer 121(1), 25–33 (2015). doi:10.1002/cncr.29010
N. Tung, J.E. Garber, A. Lincoln, S.M. Domchek, Frequency of triple-negative breast cancer in BRCA1 mutation carriers: comparison between common Ashkenazi Jewish and other mutations. J. Clin. Oncol. 30(35), 4447–4448 (2012). doi:10.1200/JCO.2012.44.5635
K.M. Kuusisto, A. Bebel, M. Vihinen, J. Schleutker, S.-L. Sallinen, Screening for BRCA1, BRCA2, CHEK2, PALB2, BRIP1, RAD50, and CDH1 mutations in high-risk Finnish BRCA1/2-founder mutation-negative breast and/or ovarian cancer individuals. Breast Cancer Res. 13(1), R20 (2011). doi:10.1186/bcr2832
S.N. Powell, L.A. Kachnic, Roles of BRCA1 and BRCA2 in homologous recombination, DNA replication fidelity and the cellular response to ionizing radiation. Oncogene 22(37), 5784–5791 (2003). doi:10.1038/sj.onc.1206678
S.F. Bunting, E. Callén, M.L. Kozak, J.M. Kim, N. Wong et al., BRCA1 functions independently of homologous recombination in DNA interstrand crosslink repair. Mol. Cell 46(2), 125–135 (2012). doi:10.1016/j.molcel.2012.02.015
M.S. Brose, T.C. Smyrk, B. Weber, H.T. Lynch, Holland–Frei cancer medicine, in Genetic Predisposition to Cancer, Chap. 16, 6th edn., ed. by D.W. Kufe, R.E. Pollock, R.R. Weichselbaum, et al. (American Cancer Society, Hamilton, 2003). doi:10.1007/978-1-62703-634-4_1
D.T. Long, J.C. Walter, A novel function for BRCA1 in crosslink repair. Mol. Cell 46(2), 111–112 (2012). doi:10.1016/j.molcel.2012.04.010
S.B. Cantor, D.W. Bell, S. Ganesan, E.M. Kass, R. Drapkin et al., BACH1, a novel helicase-like protein, interacts directly with BRCA1 and contributes to its DNA repair function. Cell 105(1), 149–160 (2001). doi:10.1016/S0092-8674(01)00304-X
M.W. Wong, C. Nordfors, D. Mossman, G. Pecenpetelovska, K.A. Avery-Kiejda, B. Talseth-Palmer, N.A. Bowden, R.J. Scott, BRIP1, PALB2, and RAD51C mutation analysis reveals their relative importance as genetic susceptibility factors for breast cancer. Breast Cancer Res. Treat. 127(3), 853–859 (2011). doi:10.1007/s10549-011-1443-0
R. Buisson, J. Niraj, J. Pauty, R. Maity, W. Zhao, Y. Coulombe, P. Sung, J.-Y. Masson, Breast cancer proteins PALB2 and BRCA2 stimulate polymerase h in recombination-associated DNA synthesis at blocked replication forks. Cell Rep. 6(3), 553–564 (2014). doi:10.1016/j.celrep.2014.01.009
N. Rahman, S. Seal, D. Thompson, P. Kelly, A. Renwick et al., PALB2, which encodes a BRCA2-interacting protein, is a breast cancer susceptibility gene. Nat. Genet. 39(2), 165–167 (2007). doi:10.1038/ng1959
W.L. Bridge, C.J. Vandenberg, R.J. Franklin, K. Hiom, The BRIP1 helicase functions independently of BRCA1 in the Fanconi anemia pathway for DNA crosslink repair. Nat. Genet. 37(9), 953–957 (2005). doi:10.1038/ng1627
P.-L. Chen, C.-F. Chen, Y. Chen, J. Xiao, Z.D. Sharp, W.-H. Lee, The BRC repeats in BRCA2 are critical for RAD51 binding and resistance to methyl methanesulfonate treatment. PNAS 95(9), 5287–5292 (1998). doi:10.1073/pnas.95.9.5287
A. Carreira, S.C. Kowalczykowski, Two classes of BRC repeats in BRCA2 promote RAD51 nucleoprotein filament function by distinct mechanisms. PNAS 108(26), 10448–10453 (2011). doi:10.1073/pnas.1106971108
S. Woditschka, D. Palmieri, R. Duchnowska, J. Jassem, S. Badve, G.W. Sledge, P.S. Steeg, Overexpression of RAD51 promotes brain metastases from breast cancer. Cancer Res. 73(8 Suppl.), 4589 (2013). doi:10.1158/1538-7445.AM2013-4589
H.L. Klein, The consequences of Rad51 overexpression for normal and tumor cells. DNA Repair 7(5), 686–693 (2008). doi:10.1016/j.dnarep.2007.12.008
J.-Y. Park, T.R. Singh, N. Nassar, F. Zhang, M. Freund, H. Hanenberg, A.R. Meetei, P.R. Andreassen, Breast cancer-associated missense mutants of the PALB2 WD40 domain, which directly binds RAD51C, RAD51 and BRCA2, disrupt DNA repair. Oncogene 33(40), 4803–4812 (2013). doi:10.1038/onc.2013.421
R. Hashizume, M. Fukuda, I. Maeda, H. Nishikawa, D. Oyake, Y. Yabuki, H. Ogata, T. Ohta, The RING heterodimer BRCA1-BARD1 is a ubiquitin ligase inactivated by a breast cancer-derived mutation. J. Biol. Chem. 276(18), 14537–14540 (2001). doi:10.1074/jbc.C000881200
D. Lisa, S. Daniela, Y.S. Simone, K. Julia, W. Lisa, BRCA1-mediated repression of mutagenic end-joining of DNA double-strand breaks requires complex formation with BACH1. Biochem. J. 441(3), 919–926 (2012). doi:10.1042/BJ20110314
R. Parsons, L. Simpson, PTEN and cancer, in Tumor Suppressor Genes Volume 1: Pathways and Isolation Strategies, ed. by W.S. El-Deiry (Springer, New York, 2003), pp. 147–166. doi:10.1385/1-59259-328-3:147
J. Li, C. Yen, D. Liaw, K. Podsypanina, S. Bose et al., PTEN, a putative protein tyrosine phosphatase gene mutated in human brain, breast, and prostate cancer. Science 275(5308), 1943–1947 (1997). doi:10.1126/science.275.5308.1943
L.-P. Weng, W.M. Smith, P.L. Dahia, U. Ziebold, E. Gil, J.A. Lees, C. Eng, PTEN suppresses breast cancer cell growth by phosphatase activity-dependent G1 arrest followed by cell death. Cancer Res. 59(22), 5808–5814 (1999)
P.L. Depowski, S.I. Rosenthal, J.S. Ross, Loss of expression of the PTEN gene protein product is associated with poor outcome in breast cancer. Mod. Pathol. 14(7), 672–676 (2001). doi:10.1038/modpathol.3880371
A. Carracedo, A. Alimonti, P.P. Pandolfi, PTEN level in tumor suppression: how much is too little? Cancer Res. 71(3), 629–633 (2011). doi:10.1158/0008-5472.CAN-10-2488
M.S. Song, L. Salmena, P.P. Pandolfi, The functions and regulation of the PTEN tumour suppressor. Nat. Rev. Mol. Cell Biol. 13(5), 283–296 (2012). doi:10.1038/nrm3330
E.-S.A. Arafa, Q. Zhu, Z.I. Shah, G. Wani, B.M. Barakat, I. Racoma, M.A. El-Mahdy, A.A. Wani, Thymoquinone up-regulates PTEN expression and induces apoptosis in doxorubicin-resistant human breast cancer cells. Mutat. Res./Fundam. Mol. Mech. Mutagen. 706(1), 28–35 (2011). doi:10.1016/j.mrfmmm.2010.10.007
A. Bononi, M. Bonora, S. Marchi, S. Missiroli, F. Poletti, C. Giorgi, P. Pandolfi, P. Pinton, Identification of PTEN at the ER and MAMs and its regulation of Ca2+ signaling and apoptosis in a protein phosphatase-dependent manner. Cell Death Differ. 20(12), 1631–1643 (2013). doi:10.1038/cdd.2013.77
M. Unseld, A. Chilla, C. Pausz, J. Breuss, G. Schabbauer, G. Prager, PTEN dependent angiogenesis is mainly regulated by (tumor secreted-) uPAR. Cancer Res. 74(19 Suppl.), 3602 (2014). doi:10.1158/1538-7445.AM2014-3602
S. Mondal, K.K. Subramanian, J. Sakai, B. Bajrami, H.R. Luo, Phosphoinositide lipid phosphatase SHIP1 and PTEN coordinate to regulate cell migration and adhesion. Mol. Biol. Cell 23(7), 1219–1230 (2012). doi:10.1091/mbc.E11-10-0889
M. Tamura, J. Gu, K. Matsumoto, S.-I. Aota, R. Parsons, K.M. Yamada, Inhibition of cell migration, spreading, and focal adhesions by tumor suppressor PTEN. Science 280(5369), 1614–1617 (1998). doi:10.1126/science.280.5369.1614
K.M. Yamada, M. Araki, Tumor suppressor PTEN: modulator of cell signaling, growth, migration and apoptosis. J. Cell Sci. 114(13), 2375–2382 (2001). doi:10.1083/jcb.143.5.1375
L. Ma, J. Teruya-Feldstein, R.A. Weinberg, Tumour invasion and metastasis initiated by microRNA-10b in breast cancer. Nature 449(7163), 682–688 (2007). doi:10.1038/nature06174
M.V. Iorio, M. Ferracin, C.-G. Liu, A. Veronese, R. Spizzo et al., MicroRNA gene expression deregulation in human breast cancer. Cancer Res. 65(16), 7065–7070 (2005). doi:10.1158/0008-5472.CAN-05-1783
L.-X. Yan, X.-F. Huang, Q. Shao, M.-Y. Huang, L. Deng, Q.-L. Wu, Y.-X. Zeng, J.-Y. Shao, MicroRNA miR-21 overexpression in human breast cancer is associated with advanced clinical stage, lymph node metastasis and patient poor prognosis. RNA 14(11), 2348–2360 (2008). doi:10.1261/rna.1034808
M.V. Iorio, P. Casalini, C. Piovan, G. Di Leva, A. Merlo, T. Triulzi, S. Ménard, C.M. Croce, E. Tagliabue, microrna-205 regulates HER3 in human breast cancer. Cancer Res. 69(6), 2195–2200 (2009). doi:10.1158/0008-5472.CAN-08-2920
F. Yu, H. Yao, P. Zhu, X. Zhang, Q. Pan, C. Gong, Y. Huang, X. Hu, F. Su, J. Lieberman, let-7 regulates self renewal and tumorigenicity of breast cancer cells. Cell 131(6), 1109–1123 (2007). doi:10.1016/j.cell.2007.10.054
R. Liu, X. Wang, G.Y. Chen, P. Dalerba, A. Gurney et al., The prognostic role of a gene signature from tumorigenic breast-cancer cells. N. Engl. J. Med. 356(3), 217–226 (2007). doi:10.1056/NEJMoa063994
Y. Lee, V.N. Kim, In vitro and in vivo assays for the activity of Drosha complex. Methods Enzymol. 427, 87–106 (2007). doi:10.1016/S0076-6879(07)27005-3
H.M. Heneghan, N. Miller, A.J. Lowery, K.J. Sweeney, J. Newell, M.J. Kerin, Circulating microRNAs as novel minimally invasive biomarkers for breast cancer. Ann. Surg. 251(3), 499–505 (2010). doi:10.1097/SLA.0b013e3181cc939f
E. O’Day, A. Lal, MicroRNAs and their target gene networks in breast cancer. Breast Cancer Res. 12(2), 201 (2010). doi:10.1186/bcr2484
S. Sethi, A. Ahmad, S. Mittal, R. Ali, W. Chen, F.H. Sarkar, Upregulation of miR-10b associated with breast cancer metastasis to brain. Cancer Res. 73(8 Suppl.), 5327 (2013). doi:10.1158/1538-7445.AM2013-5327
L.B. Frankel, N.R. Christoffersen, A. Jacobsen, M. Lindow, A. Krogh, A.H. Lund, Programmed cell death 4 (PDCD4) is an important functional target of the microRNA miR-21 in breast cancer cells. J. Biol. Chem. 283(2), 1026–1033 (2008). doi:10.1074/jbc.M707224200
P. Gasparini, F. Lovat, M. Fassan, L. Casadei, L. Cascione et al., Protective role of miR-155 in breast cancer through RAD51 targeting impairs homologous recombination after irradiation. PNAS 111(12), 4536–4541 (2014). doi:10.1073/pnas.1402604111
P.C. Gøtzsche, M. Nielsen, L. Casadei, Screening for breast cancer with mammography. Cochrane Database Syst. Rev. 1, CD001877 (2011). doi:10.1002/14651858.CD001877.pub4
E.S. de Paredes (ed.), Atlas of Mammography, 3rd edn. (Lippincott Williams & Wilkins, Philadelphia, 2007)
C.E.C. Marie Tartar, M.S. Kipper (eds.). Breast Cancer Imaging: A Multidisciplinary, Multimodality Approach (Mosby Elsevier, Philadelphia, PA, 2008)
J.G. Herman, J.R. Graff, S. Myöhänen, B.D. Nelkin, S.B. Baylin, Methylation-specific PCR: a novel PCR assay for methylation status of CpG islands. PNAS 93(18), 9821–9826 (1996). doi:10.1073/pnas.93.18.9821
A.E. Hoffman, T. Zheng, C. Yi, D. Leaderer, J. Weidhaas, F. Slack, Y. Zhang, T. Paranjape, Y. Zhu, microRNA miR-196a-2 and breast cancer: a genetic and epigenetic association study and functional analysis. Cancer Res. 69(14), 5970–5977 (2009). doi:10.1158/0008-5472.CAN-09-0236
D.C. Sgroi, S. Teng, G. Robinson, R. LeVangie, J.R. Hudson, A.G. Elkahloun, In vivo gene expression profile analysis of human breast cancer progression. Cancer Res. 59(22), 5656–5661 (1999)
S. Paik, G. Tang, S. Shak, C. Kim, J. Baker et al., Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor–positive breast cancer. J. Clin. Oncol. 24(23), 3726–3734 (2006). doi:10.1200/JCO.2005.04.7985
D. Ford, D. Easton, M. Stratton, S. Narod, D. Goldgar et al., Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. Am. J. Hum. Genet. 62(3), 676–689 (1998). doi:10.1086/301749
J.S. Reis-Filho, L. Pusztai, Gene expression profiling in breast cancer: classification, prognostication, and prediction. Lancet 378(9805), 1812–1823 (2011). doi:10.1016/S0140-6736(11)61539-0
M.A. Innis, D.H. Gelfand, J.J. Sninsky, T.J. White (eds.), PCR Protocols: A Guide to Methods and Applications (Academic Press, San Diego, 2012)
E. Evron, W.C. Dooley, C.B. Umbricht, D. Rosenthal, N. Sacchi et al., Detection of breast cancer cells in ductal lavage fluid by methylation-specific PCR. Lancet 357(9265), 1335–1336 (2001). doi:10.1016/S0140-6736(00)04501-3
M. Ignatiadis, G. Kallergi, M. Ntoulia, M. Perraki, S. Apostolaki et al., Prognostic value of the molecular detection of circulating tumor cells using a multimarker reverse transcription-PCR assay for cytokeratin 19, mammaglobin A, and HER2 in early breast cancer. Clin. Cancer Res. 14(9), 2593–2600 (2008). doi:10.1158/1078-0432.CCR-07-4758
M.J. Fackler, M. McVeigh, J. Mehrotra, M.A. Blum, J. Lange, A. Lapides, E. Garrett, P. Argani, S. Sukumar, Quantitative multiplex methylation-specific PCR assay for the detection of promoter hypermethylation in multiple genes in breast cancer. Cancer Res. 64(13), 4442–4452 (2004). doi:10.1158/0008-5472.CAN-03-3341
T. Fehm, O. Hoffmann, B. Aktas, S. Becker, E.F. Solomayer, D. Wallwiener, R. Kimmig, S. Kasimir-Bauer, Detection and characterization of circulating tumor cells in blood of primary breast cancer patients by RT-PCR and comparison to status of bone marrow disseminated cells. Breast Cancer Res. 11(4), R59 (2009). doi:10.1186/bcr2349
K. Cuk, M. Zucknick, J. Heil, D. Madhavan, S. Schott et al., Circulating microRNAs in plasma as early detection markers for breast cancer. Int. J. Cancer 132(7), 1602–1612 (2013). doi:10.1002/ijc.27799
A. Mangolini, M. Ferracin, M.V. Zanzi, E. Saccenti, S.O. Ebnaof et al., Diagnostic and prognostic microRNAs in the serum of breast cancer patients measured by droplet digital PCR. Biomarker Res. 3(1), 12 (2015). doi:10.1186/s40364-015-0037-0
S. Asaga, C. Kuo, T. Nguyen, M. Terpenning, A.E. Giuliano, D.S. Hoon, Direct serum assay for microRNA-21 concentrations in early and advanced breast cancer. Clin. Chem. 57(1), 84–91 (2011). doi:10.1373/clinchem.2010.151845
E.S. Lianidou, A. Markou, Circulating tumor cells in breast cancer: detection systems, molecular characterization, and future challenges. Clin. Chem. 57(9), 1242–1255 (2011). doi:10.1373/clinchem.2011.165068
C. Kretschmer, A. Sterner-Kock, F. Siedentopf, W. Schoenegg, P.M. Schlag, W. Kemmner, Identification of early molecular markers for breast cancer. Mol. Cancer 10(1), 15 (2011). doi:10.1186/1476-4598-10-15
T.W. Jacobs, A.M. Gown, H. Yaziji, M.J. Barnes, S.J. Schnitt, Comparison of fluorescence in situ hybridization and immunohistochemistry for the evaluation of HER-2/neu in breast cancer. J. Clin. Oncol. 17(7), 1974 (1999)
A.A. Onitilo, J.M. Engel, R.T. Greenlee, B.N. Mukesh, Breast cancer subtypes based on ER/PR and Her2 expression: comparison of clinicopathologic features and survival. Clin. Med. Res. 7(1–2), 4–13 (2009). doi:10.3121/cmr.2008.825
W. Saadi, S.-J. Wang, F. Lin, N.L. Jeon, A parallel-gradient microfluidic chamber for quantitative analysis of breast cancer cell chemotaxis. Biomed. Microdevices 8(2), 109–118 (2006). doi:10.1007/s10544-006-7706-6
H.W. Hou, Q. Li, G. Lee, A. Kumar, C. Ong, C.T. Lim, Deformability study of breast cancer cells using microfluidics. Biomed. Microdevices 11(3), 557–564 (2009). doi:10.1007/s10544-008-9262-8
K.W. Kwon, S.S. Choi, S.H. Lee, B. Kim, S.N. Lee, M.C. Park, P. Kim, S.Y. Hwang, K.Y. Suh, Label-free, microfluidic separation and enrichment of human breast cancer cells by adhesion difference. Lab on a Chip 7(11), 1461–1468 (2007). doi:10.1039/b710054j
M.J. Van De Vijver, Y.D. He, L.J. van’t Veer, H. Dai, A.A. Hart, A gene-expression signature as a predictor of survival in breast cancer. N. Engl. J. Med. 347(25), 1999–2009 (2002). doi:10.1056/NEJMoa021967
J. Knight, Microfluidics: Honey. I shrunk the lab. Nature 418(6897), 474–475 (2002). doi:10.1038/418474a
J. Chen, D. Chen, Y. Xie, T. Yuan, X. Chen, Progress of microfluidics for biology and medicine. Nano-Micro Lett. 5(1), 66–80 (2013). doi:10.1007/BF03354852
J. Chen, J. Li, Y. Sun, Microfluidic approaches for cancer cell detection, characterization, and separation. Lab Chip 12(10), 1753–1767 (2012). doi:10.1039/c2lc21273k
T.A. Nguyen, T.-I. Yin, D. Reyes, G.A. Urban, Microfluidic chip with integrated electrical cell-impedance sensing for monitoring single cancer cell migration in three-dimensional matrixes. Anal. Chem. 85(22), 11068–11076 (2013). doi:10.1021/ac402761s
J.W. Song, S.P. Cavnar, A.C. Walker, K.E. Luker, M. Gupta, Y.-C. Tung, G.D. Luker, S. Takayama, Microfluidic endothelium for studying the intravascular adhesion of metastatic breast cancer cells. PloS One 4(6), e5756 (2009). doi:10.1371/journal.pone.0005756
A.T.-H. Hsieh, P.J.-H. Pan, A.P. Lee, Rapid label-free DNA analysis in picoliter microfluidic droplets using FRET probes. Microfluid. Nanofluid 6(3), 391–401 (2009). doi:10.1007/s10404-009-0406-9
K.A. Mangold, V. Wang, S.M. Weissman, W.S. Rubinstein, K.L. Kaul, Detection of BRCA1 and BRCA2 Ashkenazi Jewish founder mutations in formalin-fixed paraffin-embedded tissues using conventional PCR and heteroduplex/amplicon size differences. J. Mol. Diagn. 12(1), 20–26 (2010). doi:10.2353/jmoldx.2010.090023
A. Rasooly, J. Jacobson, Development of biosensors for cancer clinical testing. Biosens. Bioelectron. 21(10), 1851–1858 (2006). doi:10.1016/j.bios.2006.01.003
J. van Mameren, M. Modesti, R. Kanaar, C. Wyman, E.J. Peterman, G.J. Wuite, Counting RAD51 proteins disassembling from nucleoprotein filaments under tension. Nature 457(7230), 745–748 (2009). doi:10.1038/nature07581
S. Vorwerk, K. Ganter, Y. Cheng, J. Hoheisel, P.F. Stähler, M. Beier, Microfluidic-based enzymatic on-chip labeling of miRNAs. New Biotechnol. 25(2), 142–149 (2008). doi:10.1016/j.nbt.2008.08.005
F. Moltzahn, A.B. Olshen, L. Baehner, A. Peek, L. Fong, H. Stöppler, J. Simko, J.F. Hilton, P. Carroll, R. Blelloch, Microfluidic-based multiplex qRT-PCR identifies diagnostic and prognostic microRNA signatures in the sera of prostate cancer patients. Cancer Res. 71(2), 550–560 (2011). doi:10.1158/0008-5472.CAN-10-1229
J.S. Jang, V.A. Simon, R.M. Feddersen, F. Rakhshan, D.A. Schultz, M.A. Zschunke, W.L. Lingle, C.P. Kolbert, J. Jen, Quantitative miRNA expression analysis using fluidigm microfluidics dynamic arrays. BMC Genomics 12(1), 144 (2011). doi:10.1186/1471-2164-12-144
R. Fan, O. Vermesh, A. Srivastava, B.K. Yen, L. Qin et al., Integrated barcode chips for rapid, multiplexed analysis of proteins in microliter quantities of blood. Nat. Biotechnol. 26(12), 1373–1378 (2008). doi:10.1038/nbt.1507
M. Hu, J. Yan, Y. He, H. Lu, L. Weng, S. Song, C. Fan, L. Wang, Ultrasensitive, multiplexed detection of cancer biomarkers directly in serum by using a quantum dot-based microfluidic protein chip. ACS Nano 4(1), 488–494 (2009). doi:10.1021/nn901404h
A.F.-J. Jou, C.-H. Lu, Y.-C. He, H. Ou, S.-S. Wang, S.-L. Hsu, I. Willne, J.A. Ho, Diagnosing the miR-141 prostate cancer biomarker using nucleic acid-functionalized CdSe/ZnS QDs and telomerase. Chem. Sci. 6(1), 659–665 (2009). doi:10.1039/C4SC02104E
J.S. Shim, A.W. Browne, C.H. Ahn, An on-chip whole blood/plasma separator with bead-packed microchannel on COC polymer. Biomed. microdevices 12(5), 949–957 (2010). doi:10.1007/s10544-010-9449-7
G. Perozziello, P. Candeloro, F. Gentile, A. Nicastri, A. Perri et al., Microfluidics & nanotechnology: towards fully integrated analytical devices for the detection of cancer biomarkers. RSC Adv. 4(98), 55590–55598 (2014). doi:10.1039/C4RA10486B
C.B. Moelans, P.J. van Diest, Breast: Ductal carcinoma. Atlas Genet. Cytogenet. Oncol. Haematol. 17(3), 209–220 (2012). doi:10.4267/2042/48766
R.T. Abraham, Cell cycle checkpoint signaling through the ATM and ATR kinases. Genes Dev. 15(17), 2177–2196 (2001). doi:10.1101/gad.914401
K. Yoshida, Y. Miki, Role of BRCA1 and BRCA2 as regulators of DNA repair, transcription, and cell cycle in response to DNA damage. Cancer Sci. 95(11), 866–871 (2004). doi:10.1111/j.1349-7006.2004.tb02195.x
K.K. Khanna, S.P. Jackson, DNA double-strand breaks: signaling, repair and the cancer connection. Nat. Genet. 27(3), 247–254 (2001). doi:10.1038/85798
C. Chen, D.A. Ridzon, A.J. Broomer, Z. Zhou, D.H. Lee et al., Real-time quantification of microRNAs by stem–loop RT–PCR. Nucleic Acids Res. 33(20), e179 (2005). doi:10.1093/nar/gni178